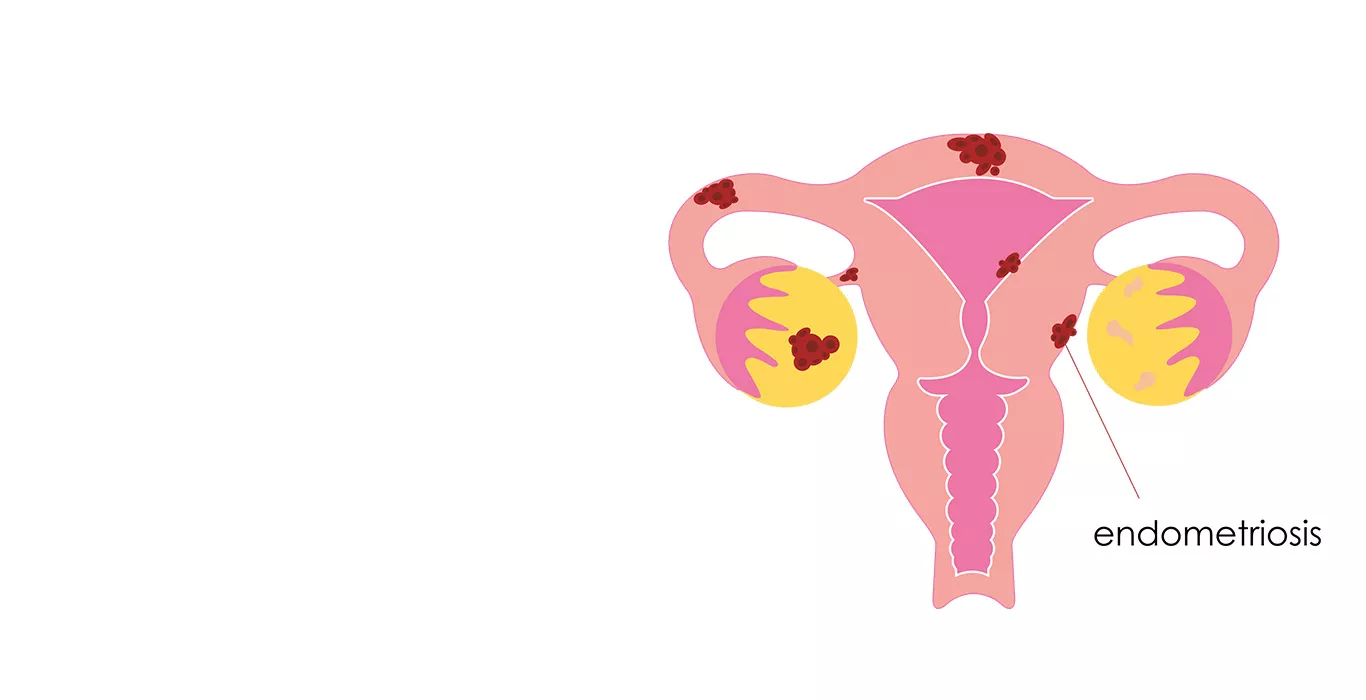
What is Endometriosis?
Endometriosis is a chronic and often painful condition medical condition that affects millions of women worldwide. In the condition, tissue similar to the lining of the uterus (the endometrium) grows outside the uterus. This tissue, called endometrial implants, can grow on various pelvic organs, such as the ovaries, fallopian tubes, and the lining of the pelvis. In rare cases, it may even spread beyond the pelvic region. Despite its prevalence, many individuals are unaware of what it is, how it develops, or how to manage it.
Who can get Endometriosis?
Endometriosis can affect women of reproductive age, typically between their early teens and menopause. It is estimated that approximately 1 in 10 women worldwide suffer from endometriosis, making it a widespread gynecological disorder.
What are the Types of Endometriosis?
Endometriosis is classified into several types based on the location and severity of the endometrial implants:
1. Superficial Peritoneal Endometriosis: This is the most common type, characterized by small, shallow implants on the peritoneum, the lining of the pelvic cavity.
2. Ovarian Endometriosis (Endometrioma): Endometrial tissue forms cysts on the ovaries, known as endometriomas or chocolate cysts.
3. Deep Infiltrating Endometriosis (DIE): In this severe form, endometrial tissue penetrates deeply into the pelvic organs, such as the rectum or bladder.
4.Adenomyosis: Although not strictly endometriosis, adenomyosis involves the invasion of endometrial tissue into the muscular wall of the uterus, causing pain and heavy menstrual bleeding.
What are the Causes of Endometriosis?
The exact cause of endometriosis remains unclear, but several theories have been proposed:
1. Retrograde Menstruation: One prevailing theory suggests that menstrual blood containing endometrial cells flows backward into the pelvis, where these cells implant and grow outside the uterus.
2. Immune System Dysfunction: Some researchers believe that immune system abnormalities may permit the survival and growth of endometrial tissue outside the uterus.
3. Hormonal Influence: Hormonal factors, particularly estrogen, may play a role in the development and progression of endometriosis. Elevated estrogen levels can stimulate the growth of endometrial implants.
4. Genetics: There is evidence that genetics may predispose some women to endometriosis, as it often runs in families.
5. Environmental Factors: Exposure to certain environmental toxins may increase the risk of developing endometriosis, although this area of research is still evolving.
What are the Symptoms of Endometriosis?
Endometriosis can manifest with various symptoms, which may range from mild to severe. Common symptoms of endometriosis include:
1. Pelvic Pain: This is the most prevalent symptom, with pain often increasing during menstruation.
2. Painful Menstruation (Dysmenorrhea): Severe menstrual cramps that can interfere with daily activities.
3. Chronic Pelvic Pain: Ongoing pain in the pelvic region, not limited to menstruation.
4. Painful Intercourse (Dyspareunia): Discomfort or pain during sexual intercourse.
5. Heavy Menstrual Bleeding (Menorrhagia): Abnormally heavy or prolonged periods.
6. Painful Bowel Movements or Urination: Especially during menstruation.
7. Infertility: Endometriosis is a leading cause of female infertility.
How is Endometriosis Diagnosed?
Diagnosing endometriosis can be challenging, as symptoms may overlap with other gynecological conditions. Diagnosis of endometriosis typically involves the following steps:
1. Medical History: Your healthcare provider will review your medical history and discuss your symptoms.
2. Physical Examination: A pelvic exam may reveal abnormalities or tenderness.
3. Imaging Studies: Ultrasound, MRI, or other imaging tests can help identify endometrial implants, especially if they are large or involve the ovaries.
4. Laparoscopy: The most definitive method for diagnosing endometriosis involves a minimally invasive surgical procedure called laparoscopy. During this procedure, a thin tube with a camera is inserted into the abdomen to visualize and potentially remove endometrial tissue for biopsy.
How is Endometriosis Treated?
The treatment of endometriosis aims to relieve pain, improve fertility (if desired), and prevent the condition from progressing. Treatment options may include:
1. Pain Medications: Over-the-counter pain relievers or prescription medications can help manage pain.
2. Hormonal Therapy: Hormonal treatments like birth control pills, hormonal IUDs, or GnRH agonists can help control symptoms by reducing estrogen levels.
3. Laparoscopic Surgery: Minimally invasive surgery can remove endometrial implants and scar tissue, improving pain and fertility.
4. Hysterectomy: In severe cases or when fertility is not a concern, a hysterectomy (removal of the uterus) may be recommended.
5.Fertility Treatments: For women who wish to conceive, assisted reproductive technologies (ART) such as in vitro fertilization (IVF).
If you suspect you have endometriosis or are experiencing any of the associated symptoms, it is essential to consult a healthcare professional or fertility expert for a proper evaluation and personalized endometriosis treatment plan.
Frequently Asked Questions (FAQs)
Can endometriosis be cured?
While there is no definitive cure for endometriosis, various treatments can effectively manage the condition's symptoms and improve quality of life.
Is endometriosis associated with an increased risk of certain health conditions?
Endometriosis may be linked to a slightly higher risk of certain health issues, such as ovarian cancer and infertility. However, the absolute risk remains relatively low.
Can pregnancy alleviate endometriosis symptoms?
Pregnancy can temporarily alleviate endometriosis symptoms for some women, likely due to hormonal changes during pregnancy. However, symptoms may return after childbirth.
Is there a link between endometriosis and autoimmune diseases?
Some studies suggest a possible connection between endometriosis and autoimmune disorders, but further research is needed to establish a definitive link.
Can lifestyle changes or dietary modifications help manage endometriosis symptoms?
Some women report symptom improvement with dietary changes and lifestyle modifications, such as reducing inflammatory foods, managing stress, and regular exercise. However, individual responses vary, and it's essential to consult a healthcare provider for a tailored approach.
Pregnancy Calculator Tools for Confident and Stress-Free Pregnancy Planning
Get quick understanding of your fertility cycle and accordingly make a schedule to track it
Get a free consultation!